| |
| |
| Bladder Control Problems |
|
|
Millions of people experience bladder control problems (BCP) and unfortunately many of these people feel like it is simply a part of getting older. The good news is that you are not alone. This is a medical problem and nearly everyone can be helped. The following information should help you discuss this condition with your urologist and understand what treatments are available to you. |
| |
|
What are bladder control problems? |
|
|
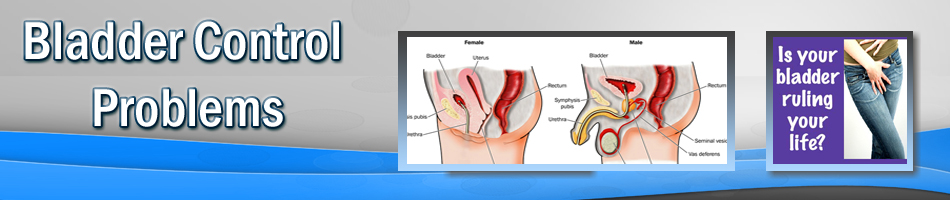
The bladder is a hollow, balloon-shaped organ that is located within the pelvis. It has two major functions: storage and emptying of urine. BCP consist of conditions that affect either function of the bladder. BCP causes a significant amount of problems affecting the quality of life of a person. Among the problems of bladder control are urinary incontinence, frequency and urgency of urination and difficulties emptying the bladder. In general, these problems are related to one or both bladder functions. For example, frequency and urgency are generally related to a bladder that cannot hold the urine to its expected capacity. The expected maximal capacity of the bladder for an adult is about 10 to 15 ounces. Difficulty emptying the bladder involves conditions such as a weak flow of urine, frequent urination and not emptying to completion. The occurrence of BCP increases with aging in both sexes. It should be emphasized, however, that BCP should not be considered "normal" as a majority of aged people do not have BCP. |
| |
|
| What are the causes of bladder control problems? |
|
|
Bladder control is regulated by interaction between the central nervous system (brain and spinal cord) and organs of the lower urinary tract (bladder, urethra, pelvic floor muscles). Therefore, any disease that involves any part of this control mechanism could affect bladder function, and thereby present itself as BCP. For example, patients with diseases that involve the central nervous system, such as neurogenic problems in children, spinal cord injuries, Parkinson's disease, cerebrovascular accidents (strokes) and multiple sclerosis, could have bladder control problems. In addition, trauma, irradiation and other injuries to the lower urinary tract and pelvic organs could potentially cause BCP. Pregnancy and vaginal delivery are considered among the risk factors for BCP.
Sometimes extra weight can cause BCP by putting extra pressure on the pelvic floor muscles. However, the majority of people with BCP have no clear symptoms of any neurological diseases or apparent damage to their lower urinary tract system.
|
| |
|
| How common is BCP? |
|
|
BCP affects both men and women at all stages of life. In the earlier stages of life BCP may be seen with congenital anomalies involving the nervous system or tissues of the pelvis and lower urinary tract. For example, patients born with spina bifida have significant problems with bladder control. A good portion of bladder function relies on bladder training during the earlier stages of life. Improper or delayed toilet training may be a symptom of BCP during the earlier stages of childhood or later in life.
|
| |
|
| What are some risk factors for BCP? |
|
|
Risk factors related to BCP happen around the childbearing ages, when the process of pregnancy and a vaginal delivery can affect bladder control. However, this problem usually goes away in the majority of patients with BCP during pregnancy or immediately after childbirth. The next series of events in life affecting BCP are around the time of menopause for women, and enlargement of the prostate in the fifth and sixth decades of life in men. Enlargement of the prostate gland occurs in the majority of the men living in the western society and may affect bladder function. Menopause can also affect bladder function. The other independent event affecting bladder function is aging and the changes that occur within the tissues of the lower urinary tract and the bladder itself.
Given that the above risk factors could affect almost everyone living in the western society, it is estimated that up to 50 percent of women and 30 percent of men will have bladder control problems during their lifetime.
|
| |
|
| What can be done for BCP? |
|
|
|
Despite the high rate of BCP, it is also known that a small number of patients with BCP seek medical attention. Although not clearly known, it is believe that most people view BCP as tolerable or a normal part of life. Nonetheless, it is clear that effective therapies (both medical and surgical) now exist which could make BCP more bearable for the majority of patients. You should talk with a urologist to learn about what treatment(s) may work best for you. |
| |
|
| How can I tell if I may have BCP? |
|
|
Given the wide range of differences among individuals, it is difficult to draw a certain line between "normal" vs. "abnormal" bladder function. It is generally agreed, however, that any symptoms of the bladder or its control that bother the person or interfere with normal lifestyle should be considered "abnormal." Given this definition, a general rule of thumb is that any aspect of bladder function is bothering a person, they should seek medical care for their BCP. Problems, such as urinary incontinence, difficulty emptying the bladder or other signs of BCP, should not be tolerated and expected as a part of normal living.
The common symptoms of BCP are: leakage of urine resulting from a cough, sneeze or physical activity, or urgency and lack of desired control to hold urination. In addition, symptoms such as frequency of urination (more than eight to ten times per day) or waking up to go to the bathroom more than twice a night, have been considered as "abnormal urinary habits." Given the fact that the symptoms of BCP could signal the presence of other conditions, such as multiple sclerosis and diabetes, attention should be paid to such symptoms. |
| |
|
| |
|
| |
|
|
 |
Endoscopic removal of urinary stones: PCNL, URS, RIRS, CLT |
|
 |
Lithotripsy (ESWL) |
|
 |
LASERS for stones and Prostate |
|
 |
Monopolar and bipolar TURP |
|
 |
HOLEP |
|
 |
Urodynamics and uroflowmetry |
|
 |
Laparoscopic urology surgeries |
|
 |
Paediatric urology surgeries |
|
 |
Urinary incontinence surgeries |
|
 |
Surgeries for genitourinary cancers |
|
 |
Reconstructive urology |
|
 |
Microsurgeries for infertility and impotence |
|
| |
|
| |
 |
|